STRETCH-OB
STRETCH-OB
This video shares what you need to know about our STRETCH-OB Program.
Structured Training for Rural Enhancement of Community Health in Obstetrics (STRETCH-OB)
STRETCH-OB is a track within our Family Medicine Residency Program for residents who are committed to providing obstetrics in a rural or underserved community. This is a HRSA-funded program and a collaboration between the University of Illinois College of Medicine Rockford’s Department of Family and Community Medicine and the Department of OB/GYN at UW Health SwedishAmerican Hospital and Crusader Community Clinic, as well as our rural partners. The purpose of the program is to reduce poor maternal and birth outcomes in rural and underserved areas by increasing the number of family medicine physicians with high-quality, evidence-based obstetrical skills who practice in these areas.
Residents participating in this track will complete all of the requirements for board certification in family medicine as well as additional obstetrics and gynecology rotations (and call) to enhance their obstetrical skills. Upon completion of their three-year residency program, STRETCH-OB residents will have experience in higher-risk obstetrics and surgical obstetrics by completing a minimum of 50 C-sections as first assist, 50 C-sections as primary surgeon and 100 vaginal deliveries.
STRETCH-OB CURRICULUM
Eligibility
- Medical school graduation within one year of start date or recent clinical activity in the practice of medicine
- Competitive applicant with demonstrated interest in practicing family medicine
- Strong interest in obstetrics with an interest and aptitude for surgical obstetrics
- Intent to practice in a rural or underserved community upon completion of residency training
These criteria are simply the requirements needed for your application to be reviewed; they do not guarantee an interview. Interviews will be granted upon further review of the application and all of its contents.
Application Process
To apply to the STRETCH-OB program, first complete the application through AAMC ERAS system indicating your interest in the University of Illinois College of Medicine Rockford Family Medicine Residency Program (#2268120C0). As part of the AAMC ERAS application, you should submit one letter of recommendation from your Department of Family Medicine, one letter from your Department of Obstetrics & Gynecology, and a third supporting letter from Family Medicine or Obstetrics.
After submitting your application through the AAMC ERAS system, please submit a letter of interest via email to STRETCH-OB@uic.edu addressing the following:
- Your interest in family medicine
- Your interest and desire to train in advanced obstetrics, including surgical obstetrics
- Why you aspire to practice in a rural or underserved area
Your letter of interest should include your name and AAMC ID # as the header. Font size should be no smaller than 10 and the letter should be no more than two pages in length.
We will contact you if we wish to schedule an interview. Interviews will take place from late October through January.
STRETCH-OB Program
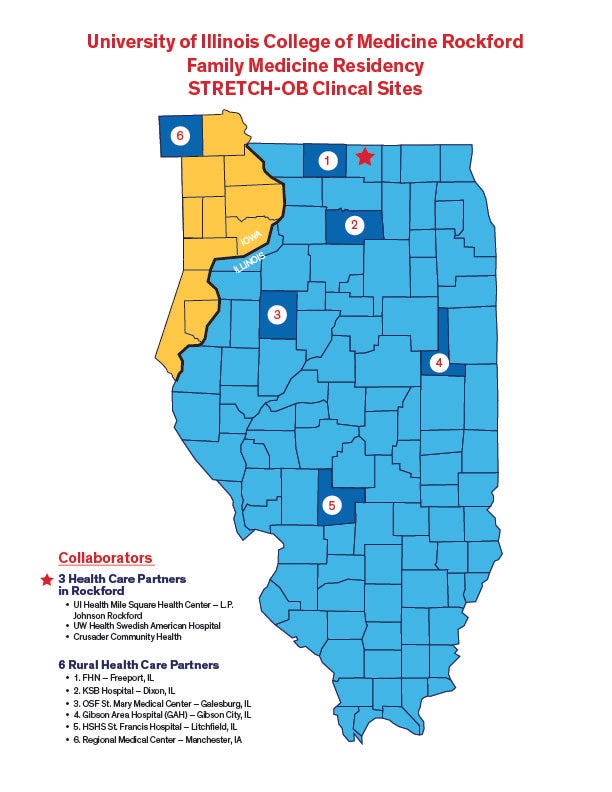
STRETCH-OB residents will complete a minimum of 50 C-sections as first assistant, 50 C-sections as primary surgeon and 100 vaginal deliveries. Residents will participate in a rural rotation as a family medicine provider of obstetrics care for one month in each of their PGY2 and PGY3 years and a rural gynecology rotation in their PGY3 year.
These rotations can be selected from our rural partner sites, Gibson Area Hospital (Gibson City, IL), Katherine Bethea Shaw Hospital (Dixon, IL), Freeport Health Network (Freeport, IL), Regional Medical Center (Manchester, IA), HSHS St. Francis (Litchfield, IL) or OSF St. Mary Medical Center (Galesburg, IL).
STRETCH-OB residents will take an additional 1-2 STRETCH-OB shifts per week when residents are not on an inpatient medicine, OB or away rotation for longitudinal C-section and delivery training.
OB Table
| Year | Program | Curriculum Comparison |
|---|---|---|
| PGY1 | Family Medical Residency Program |
|
| STRETCH-OB Program |
|
|
| PGY2 | Family Medical Residency |
|
| STRETCH-OB Program |
|
|
| PGY3 | Family Medical Residency Program |
|
| STRETCH-OB Program |
|
Accordion Section
OB Inpatient Rotation
Existing OB Curriculum plus:
- Performing C-sections as assistant and primary surgeon
- D&C, uterine sharp curettage
- Operative vaginal deliveries
- Repair of all obstetric lacerations
- Postoperative OB care
- Sterilization at the time of C-section
- External cephalic version
- Delivery of multiple gestation deliveries
- Vaginal breech delivery
- Inpatient antepartum care
- Management of common complications of pregnancy
- Management of obstetrical emergencies
Coverage
Existing OB Curriculum plus: With a complement of six family medicine residents in the STRETCH-OB program, an effort is made to provide full coverage on L&D Monday-Friday from 0700-2300, while protecting time for clinic and maintaining our full and rigorous commitment to the general family medicine training.
Other Rotations
Existing OB Curriculum plus:
- 1-month MFM in R1
- 2 – one month Rural rotations (one in R2 and one in R3)
Didactic Sessions
Existing curriculum plus: Didactics will include a full spectrum of topics in enhanced OB including preconception counseling, routine and “at risk” prenatal care, surgical obstetrics, postpartum and postoperative care, complications of pregnancy, contraception and sterilization procedures.”
Multidisciplinary OB Simulations Including Didactic
Existing OB curriculum plus:
- Assist with instruction in R3
Objective Structured Clinical Exam (OSCE) Specific to O
Existing OB curriculum plus:
- 3 additional –OSCEs; one in R2 and two in R3
Skills Training
Existing OB curriculum plus:
- Introduction to Telehealth in R1
- ALSO instructor training
Workshops
Existing OB curriculum plus:
- Participate in colposcopy and suture workshop in R2
- Assist with instruction of colposcopy and suture workshops in R3
Outpatient Prenatal Care - FQHC
Existing OB curriculum plus:
- Limited OB ultrasound
- Antenatal testing
- Manage At Risk OB Clinic
- Telehealth prenatal care
Educational Review Sessions
Existing OB curriculum plus:
- CME- OB topics in R1-R3 years
- Online modules for PPH and HTN
Community Partner Collaborative Sessions
Existing OB curriculum into the R3
- Present cases at M&M
Current Residents
Faculty
Section 7
This project is funded by the U.S. Department of Health and Human Services, Health Resources and Services Administration (USDHHS/ HRSA), Primary Care Training and Enhancement‐Community Prevention and Maternal Health grant, Grant number T3442148.